
Lameness
This paragraph describes the aspects related to lameness in elephants. Lameness is a visible disruption of the normal locomotion. Observation of the gait and resting behavior are important. It is therefore advised to make videos from the different locomotion tests that will be performed during the clinical examination. Replaying such a video in slow motion can facilitate making the proper diagnose and also makes it possible to share data with colleagues if additional consultation is useful. Smartphones are very useful for this purpose.

African elephant showing signs of lameness.
Lameness: Diagnostic procedures
Although lameness is considered the most important clinical sign of musculoskeletal disorders in other species, elephants have been shown to rarely express distinct lameness patterns. This might even be the case in severe lesions. Nevertheless, elephants do express specific alterations in their posture indicative of musculoskeletal disorders. These alterations are visually perceptible for the experienced observer (Schiffmann 2021).
To diagnose lameness it is important to know the normal locomation of an elephant. This is described in detail in the corresponding chapter. Any abnormal form of locomotion should be regarded is lameness. Usually lameness is a signal from the elephant that it is suffering of pain. However, abnormal anatomic abberations can also lead to lameness, which not always necessarily leads to pain responses (e.g. slight difference in leg length). If the elephant lifts it head during walking, special attention needs to be paid to the front legs, as this head movement may be usied as an extra manner to bring a painful leg forward.
To find out the reason why an elephant displays abnormal locomotion, the clinician needs to follow the following diagnostic steps:
-
Observe the locomotion while the elephant is walking straight from left to right and from right to left, towards the observer and away from the observer, in a left circle and in a right circle.
-
A numerical rating scoring system as described by Turner e.a. (2023) can be a useful tool to evaluate the lameness. A 4-point scale with the following numerical values for each leg was used in this study: 0=clinically sound, 1=stiffness, 2=abnormal tracking, and 4=reluctance to bear weight. The maximum total score per leg is 7 (28 for all 4 legs).
-
Observe the elephant's posture when it is in rest. For more background information about abnormal posture click here.
-
General clinical examination.
-
Check the pads and nails of all feet for cracks, tears, swelling and pain reaction on deep palpation. Try to evaluate the joints by palpation (temperature, swelling pain reaction during deep palpation) and bending/stretching on command.
-
Thermography.
-
Radiography. Click here to read about radiography of the elephant's foot. Depending on the power of the X-ray equipment, joints higher up in the leg can be visualized. Digital equipment greatly improves the image quality.
-
Full blood tests: hematology and chemistry.
Walking the elephant from left to right and vice versa will make clear if the elephant is making long steps: the hind foot needs to step into the footprint of the front foot on the same side. It also allows to observe the joints: all joints of each leg should be bent and stretched during every step the animal makes.
The rhythm of the steps should be regular. If the elephant feels pain in its right front leg, it will not support on that leg as long as will support on its healthy left front leg. What the observer will see, is that the elephant "falls" on its healthy leg. Usually this is a sign of "weight-bearing lameness". This form of lameness is usually associated with sole lesions (foreign body, abscess), fracture and the acute phase of osteoarthritis.
The second form of lameness is "movement-restricted lameness", which is seen as stiffness in one or more joints and shortening of the steps made by the affected leg (and mostly in the other legs too). This type of lameness is seen in joint and muscle problems.
Most lameness cases, however, are a combination of both forms.
The gallery below shows several examples of lameness in Asian and African elephants.


Asian elephant displaying several forms of lameness, filmed at normal speed and in slow motion. The animal can bend the joints of the left front leg and puts a lot of its body weight on that leg. At the same time, it lifts both left legs almost simultaneously ("pacing") in contrast to its left legs. The right carpal joint is completely stiff and to bring the right front leg forward, the animal has to bring it in abduction. The right hind leg is lifted abnormally when making a step forward with this leg. Nevertheless, this leg is placed in the footprint og the right front leg (normal), while the left hind legs makes too short steps. The lameness in this elephant was most likely due to multiple degenerative osteoarthritis.

35-yrs-old Asian zoo elephant with signs of severe lameness. All steps of the hind legs land in or even anterior to the footprint of the corresponding front leg. The joints of all but the right hind leg are bending and stretching normally. The knee joint of that leg is stiff. The time during which the right hind leg is on the ground is significantly shorter than that of the other 3 legs. In order to bring the right hind leg forward, the elephant needs to abduct it, lift it by lifting the right part of the pelvis at the same time. No other details about this elephant are known. This elephant may have had a fracture of the right humerus or the pelvis.

28-yrs-old Asian zoo elephant with signs of severe lameness in its right front leg. All steps are shortened. When this condition did not improve after prolonged treatment with several pain killers (NSAIDs and opiates) the elephant was humanely euthanized. At necropsy multiple joints showed severe degenerative osteoarthritis as well as an old, partly healed fracture of the right ulna.

45 yrs-old African zoo elephant with a stiff, left front leg. This leg is brought forward by swaying it in abduction. All steps are shortened and the head is sometimes slightly lifted when the left front leg is swayed forward. NSAIDs were provided but not really with the desired effect. As this condition persisted for a prolonged period, chronic degenerated osteoarthritis is the most likely cause of this lameness.

Asian zoo elephant with a stiff, slightly swollen right front leg. This leg is brought forward by swaying it somewhat in abduction. All steps are shortened. According to the zoo staff, this condition disappeared after a period of conservative treatment (reduction of movement periods). The cause of such a temporary lameness could be muscle trauma (e.g. by a blow from a herd mate) or early degenerative osteoarthritis.

Asian elephant with very stiff, legs, especially the right front leg (movement-restricted lameness). After bringing this leg forward, the animal "falls" on this leg, which means that supporting on the left front leg is painful, despite the apparently better movement of the joints of that leg (weight-bearing lameness). The distal joints of both hind legs are also limited in their movements, reflecting in shorter footsteps.


African elephant displaying joint instability in the carpal joints of both front legs. When the feet are placed on the ground, the distal parts of the legs show a valgus position.
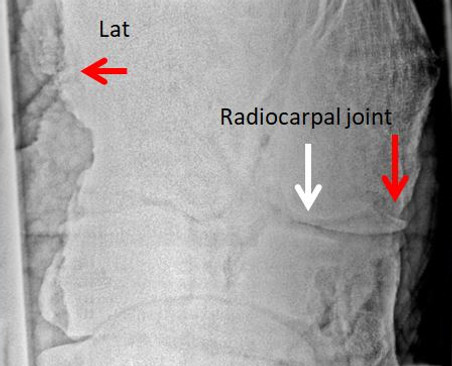

Radiographs taken from the same African elephant demonstrated periostal reaction 10-12 cm above the carpal joint, an osteophyte (spur, right red arrow) in the radiocarpal joint (osteoarthritis). The image to the right represents the carpal joint of a healthy African elephant.
The first thermography image shows a hot area at the level of the knee joint (upper arrow), suggestive for the presence of an inflammatory proces in that area. The lower arrow indicates another large hot spot. This Asian elephant was used for carrying tourists for many years in Nepal and was chained when she was not at work. The second thermography image shows a high temperature in the area of the right elbow in an Asian elephant with a swollen right front leg, also suggestive for a n inflammation of the joint (Images: courtesy of Susan Mikota).


Degenerative osteoarthritis/
Degenerative Joint Disease (DJD)
Degenerative osteoarthritis or degenerative joint disease (DJD) is quite common in elephants of advanced age. Factors that contribute to DJD are:
-
Local infection (e.g. from nail abscess)
-
Poor quality bedding substrate, no comfortable resting possibilities (sand heap)
-
Generalized infection: Mycoplasma have long been mentioned as cause of DJD because it involves multiple joints, often has a shifting lameness (Clark, 1980).
-
Rheumatoid arthritis has also been mentioned without any scientific evidence. However, lack of evidence does not necessarily exclude this form of joint disease. In humans aggravation of rheumatoid symptoms is often correlated to humidity and low temperature. As some keepers have seen a correlation between these environmental factors and pain signals of the elephant, both environmental conditions can better be avoided for elephants kept in captivity.
DJD is a chronic arthritis, characterized by loss of healthy cartilage, abnormal synovia, and irregular outline of the joint bones. Cartilage acts as a soft buffer between the bones bordering a joint. When that protective layer becomes thin or has gone, the surface of the bones are exposed to each other, which is the major cause of the pain that is experienced in DJD.
In the early phase, the area around the affected joint may be warm. In chronic cases (the majority that is seen by clinicians), the temperature is often normal or even lower than the surrounding area.

Synovia is a yellow, viscous, thread-pulling liquid, produced by the joint cartilage (see photo below). It makes it possible for the joints to articulate smoothly. If the cartilage becomes diseased, it will form abnormal synovia with a much lower viscosity (see video below; BBC).


The diagnosis of DJD is based on:
-
Symptoms as described above. Some of the following symptoms will be present: lameness during walking, abnormal position in resting position, swollen joint.
-
Locomotion test: see diagnostic procedures above.
-
Palpation: warm joint, painful joint on deep palpation)
-
Thermography: if the affected joint is warm, it will show in the thermographic image as a hot spot.
-
Radiography: DJD can only be visualized in the smaller joint (digits, carpus, tarsus). More proximal joints are hard or impossible to visualize by X-ray. Affected joints can show a smaller joint space, irregular outlines of the bones (exostosis), osteolysis, dislocation or bone fusion (ankylosis).
-
When an infection of the joint is suspected, aspiration biopsy from the affected joint should be considered for culture and antibiogram and evaluation of the synovia. However, one should be well aware of the risk to introduce an infection.


Radiograph and post-mortem photo of the hind foot bones taken from a 21 yrs-old Asian elephant with DJD involving multiple joints. Exostosis and reduced joint space can be seen on the radiograph. At necropsy the ankylosis of the digits and tarsal bones explain why the elephant was unable to bend the joints of his feet.

Positive reinforcement training made it possible to provide physiotherapy to an African elephant. Courtesy San Diego Zoo

African elephant resting its head on a tree. https://geogypsytraveler.com/wp-content/uploads/2014/01/09-028-Elephant-rest-against-a-tree-Kruger-NP-SA-gfb-knp-fff44-1024x678.jpg
TREATMENT OF DEGENERATIVE JOINT DISEASE
Acute phase:
-
Rest
-
Head rest*
-
Proper substrate (dry sand)
-
Sand pile for sleeping at night
-
Pain management
-
Corticosteroids: maybe in acute phase? [Dexamethasone (1mg/5 kg BW); Prednisolone (1mg/3 kg BW)]
Chronic phase:
-
Head rest* and sand piles
-
Physiotherapy: opportunities for walking exercises, unlimited free access to hydrotherapy (swimming pool)
-
Pain management
-
Weight reduction (if applicable)
-
Correction of abnormal pressure on foot pads
-
Monitor the condition of the lameness on a daily mobility score chart.
Pain management:
NSAID’s in acute phase (for 5 days as a start) and whenever needed in chronic cases:
-
Firocoxib 0.1 mg/kg BW PO/day (tablet or paste)
-
Meloxicam (0.03 mg/kg BW PO/day)
-
Flunixin (1,1 mg kg BW, PO/IM/IV, BID)
-
Ibuprofen (6 mg/kg BW PO, BID)
-
Phenylbutazone (4,4-8,8 mg kg BW PO/day)
Opiates: tramadol (0.5mg/kg PO BID) – combined with NSAID
Some of the anecdotally reported treatments for DJD are:
-
Physiotherapy: 2x30 minutes/day walking in figure 8 rounds, walking over small steps.
-
Hydrotherapy
-
Laser
-
Glucosamine/chondroitin
-
Gabapentine (anti-epileptic drug, 1.5mg/kg BID)
-
Acupuncture
-
Stem cells

The provision of sand piles is essential for the prevention and treatment of joint problems
Correction of unequal leg length:
One report describes the use of a rubber sole to correct the abnormal positioning of the right front leg of an Asian elephant, caused by unequal leg length. A thick multiple-layer rubber sole was glued underneath the pad of the animal (figure below A and B) (Johnson 2018). A liquid urethane glue (also used in horses) kept the pads in place for 4 weeks. The elephant was provided with bilateral wedge pads to offload pressure from the fourth nails (C).
A rubber sole can probably also be used to protect a very thin sole with a compression sore.
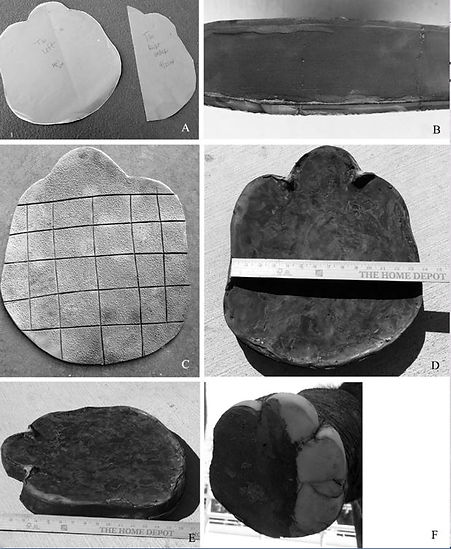
Elephant glue-on shoe construction and materials. A. Paper pattern pieces for a whole foot shoe (left), and a partial wedge (right). B. A view of the side of the wedge showing the multiple layers of rubber soling material sandwiched together. C. Shoe bottom with checkerboard tread. D. Top of a used shoe. E. Another view of the shoe showing the medial height. F. Elephant wearing the oblong wedge pad on the bottom of the right foot.

Elephant posture standing, before and after shoes.
A. Elephant leaning on the left front foot
because of asymmetry in leg length before shoes were applied. B. Elephant wearing shoes and standing square. C. Close-up of partial wedge pad on right foot (arrowheads) and elevated shoe on left foot.
* Especially in case of joint disease in the fore legs, reducing the weight on these legs is a great relieve to the elephant, as the fore legas and the head form 60% of the total body weight of the elephant. A head rest is just an elevated bar, where the animal can put its head on. Any surface that is strong enough to hold the weight of the head adjusted to the right hight may relieve the pain caused by degenerative joint disease.
Muscle-related problems
Wound, abscess
Lameness may be seen when muscles are involved in (local) infection or traumatic injury. A local infection can be caused by any perforation of the skin by and injection, arrow, gun shot, etc. This may result in abscess formation. When the elephant ahs to sleep on a concrete floor, it may develop a compression sore, that can affect the underlying muscles.
Treatment of this kind of lesions includes:
Creation of draining
Removal of the foreign body
Daily flushing of the wound with saline and mile disinfectant (e.g. diluted Betadine or chlorhexidine).
In severe cases a systemic antibiotic might be indicated (after culture and sensitivity test)
Black leg (Clostridium chauvoei or C. septicum
This bacterial infection is described on the web page: Clostridiosis. Click here for further reading.
Capture myopathy
Capture myopathy or exertional stress is a condition is characterized by severe lameness of all 4 legs. It is caused by a complex alteration of metabolic processes usually associated with capture, transport, restraint or work overload (timber industry). The acid-base and electrolyte balances are disturbed, which results in an acute lameness. It becomes fatal when the heart muscle is affected. The urine turns dark brown due to the presence of myoglobine that is the result of muscle necrosis (see photo). In some less severe cases and when the animal is treated adequately the muscle damage can be limited and the animal may survive.

Treatment of capture myopathy:
-
Absolute rest
-
Deep sand layer on floor
-
NSAID’s
-
Easy-chewable forage, chopped
-
Darkened environment
-
Long-acting tranquilization
Tendon laxity
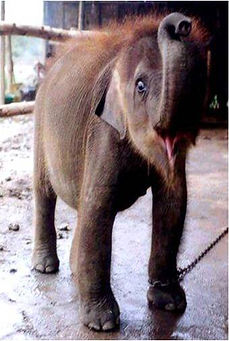
Tendon laxity (or flexural deformity) refers to a disorder that causes weak flexor tendons. It is not uncommon in newborn horse foals, especially premature ones. This condition usually fixes itself with controlled exercise. The orphan African elephant on this photo seems to suffer a similar condition. The outcome of treatment exercises remained unknown, as the elephant died of non-related problems.

Tendon contracture (arthrogryposis)
An assumed arthrogryposis was found in a stillborn calf that was delivered by fetotomy after a retention period of 13 months. Both carpal joints were firmly fixated in bent position. Stretching of the joint was only possible after cutting the flexor tendons (as done in the left front leg of the calf on the photo). Click here for the case report.

Neurology-related lameness
Tetanus
Elephants are susceptible to Clostridium tetani. Similar to exertional myopathy, the affected elephant will have stiff legs. External stimuli will result in excitation and aggravation of the muscle contractures. For further reading click here.
Botulism
Botulism is a paralytic disease caused by the toxines of Clostridium botulinum. In elephants it was first reported in 1962 in a German zoo (Elze, 1962). The diagnosis was based on the successful treatment of the paralytic lameness by the timely administration of botulism antitoxines.
In another outbreak 5 out of a group of 6 Asian elephant bulls died of botulism in the course of a few days. It started with a general weakness that became progressively worse. Shivering and mild salivation preceded the inability to stand and properly use of the trunk. For further reading click here.
Nutrition-related lameness
Metabolic bone disease
Metabolic bone disease (rickets, secondary nutritional hyperparathyroidism) has been reported in very young hand-raised elephant calves. It is a caused by an absolute deficiency of nutritional calcium (and vitamin D?), and a imbalance or lack of other minerals (e.g. phosphorus, magnesium) and proteins. There is no evidence about the potential involvement of vitamin D3 deficiency. Elephants up to the age of 9 months are susceptible to this condition, basically during the period that they should be on a 100% maternal milk diet. During lactation the fat concentration in the mother milk increases together with the calcium level (Abbondanza, 2013). This means that the calcium concentration in milk replacers must be increased as the calf grows older.
Asian elephant calf with a distinct swelling in the left elbow region. Note the abnormal posture of the left front leg (Courtesy: Susan Mikota).

Radiograph showing pathological fractures consistent with secondary hyperparathyroidism (Courtesy: Charles Reid in: Fowler en Mikota, 2006).
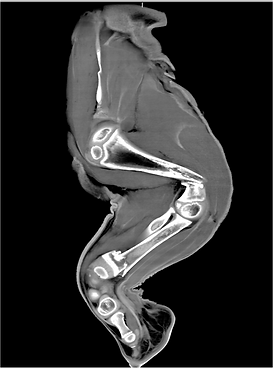

As demonstrated by the CT-scans on these photos, the demineralisation of the growing bones will lead to pathological fractures: one fracture in the distal humerus and one fracture in the distal radius. (Photos of the CT-scans were kindly provided by the Leibniz Institute for Zoo- and Wildlife Research).
Treatment and prevention of metabolic bone disease is based on maintaining the right diet (fat, proteins, Ca, P, Mg, vitamin D) and monitoring the blood total and ionized calcium levels, as well as phosphorus and magnesium. It is also recommended to make X-rays of the long bones of the growing calf on regular intervals (2-3 months) to check the bone quality and shape. Sufficient exercise of the hand-raised calf is very important for the development of a strong skeleton.
Bone fractures
Despite the solid consistency of elephant bones, fractures are not uncommon. Fractures always result in weight-bearing lameness as is clearly demonstrated on the video of the young Asian elephant bull with a fracture of the radius and ulna (Courtesy Dak Lak Elephant Conservation Center). The animal was hit by an adult female. As the distal part of the elephant's foot is missing, it was not possible to apply a splint. Possibly the shortage of the affected leg worked to his advantage, as he was able to walk on 3 legs until the fracture ends had healed.

Radiographs taken from the same young Asian elephant. Note the spiral shape and dislocation of the fracture ends of the radius and ulna. The bones healed completely within a 3 months period.


Several types of casts and bandages have been tried in elephants that had a fractured leg. Some of them are displayed below.
An adult Asian elephant presented at the Lampang Elephant Conservation Center-Thailand with a fracture and dislocation of the left fibula (see radiographs). A cast was made locally, which remained in place for the next 5 months. During this period the elephant stayed with the owner and the cast was changed 3 times.
Photos courtesy: Taweepoke Angkawanish





This adult Asian elephant was also presented at the Lampang Elephant Conservation Center-Thailand. A fracture of the tibia was suspected and a splint was made just to assist the elephant by reducing full the weight on its affected leg.
Photo courtesy: Taweepoke Angkawanish
At Pinnawala Elephant Orphanage (Sri Lanka) a radius and ulna fracture in a 2-yrs-old Asian elephant was treated by the application of a Robert Jones bandage and a fiberglass cast (Karunarathne, 2017). The bandage and cast were renewed twice. Several sedations were required to put the cast in place. Two weeks after the 3rd cast was fixed, the calf succeeded in removing it, but at that time it was able to put weight on the affected leg with a mild limp.


To reduce the pressure on fractured bone ends, it may be helpful to provide a sling in which the elephant can be supported while standing. This is only an option if the elephant is accepting such a device, which needs to be located in a trusted environment outside the reach of other, non-friendly elephants. Some improvisation skill to make such a construction will by useful. It can also be used in elephants that have a joint dislocation or other conditions in which weight reduction on one leg is required.

Photo courtesy: Susan Mikota
Hydrotherapy
Many attempts to treat major bone fractures in elephants have failed, largely due to the animals’ immense body weight. To date, no scientific reports have documented the use of hydrotherapy in such cases. However, at the 19th International Elephant Conservation and Research Symposium of the International Elephant Foundation (Chiang Mai, 2023), Dr. K.K. Sarma, Head of the Department of Surgery and Radiology at the College of Veterinary Science in Guwahati, India, presented several cases of leg fractures in semi-wild and free-ranging Asian elephants. Remarkably, these elephants appeared to choose hydrotherapy on their own, spending extended periods—sometimes several weeks—in water bodies such as lakes or large pools. They would typically emerge only once a day to forage. No splints or orthopedic devices were applied, yet the healing outcomes were striking.
Joint dislocation
Traumatic joint dislocations have been reported anecdotically.
A 3-yrs-old orphan Asian elephant was found in a range country after a bushfire. It was noticed that its right front leg seemed longer than the left one. It was brought up in a zoo in Asia and moved to Europe to become integrated in the EAZA breeding program. Is he grow older, the asymmetry of his front legs worsened and he developed a significant weight bearing and movement-restriction lameness. During locomotion he swayed his right front leg forward.
The bull was mildly sedated and examined in a restraint chute. Ultrasonographic examination revealed excessive fluid in the right elbow joint. Radiography failed due to the large size of the animal. To check the stiffness of the left elbow joint, a long rope was tied to the left carpus while in left lateral recumbency. Three individuals tried to stretch that leg; during this attempt, a clear crack was heard while the joint stretched only a few degrees. It was concluded that the joint was severely damaged and partial ankylosis had taken place. The elephant was humanely euthanized.
At necropsy a ruptured joint capsule and ruptured ligaments of the right elbow were found. The cartilage showed multiple defects, exposing the underlying bone.


Another traumatic joint dislocation was reported from Myanmar (Ann-Kathrin Oerke, 2022). An adult bull got its left hind leg stuck between the fork formed by two trees when it fell down. The capsule and ligaments of the tibio-tarsal joint ruptured and the distal part of the tibia perforated the skin. Treatment was no option and the animal died under miserable circumstances.


Severe traumatic leg injuries
Too many elephants have suffered traumatic leg injuries due to mine explosions, snares and other forms of poaching. In recent years partial leg amputation has been practiced with some success in Asian range countries. In most cases a prosthesis is needed to enable the elephant to walk.
Missing all toes of front leg
A 3-4 yrs-old wild Asian elephant bull was found with an old injury on its left front leg. All toes were missing and there was a deep wound on the palmar side of the remnants of that foot. A circular scar was visible about 15 cm from the "pad"; 4 small fistulas were located in the line of this scar, each of them oozing thick purulent exudate. Most of the time (70-90% the animal displayed stereotypical behavior: touching the remnant of its left foot and beating it with its trunk.



The animal was brought to a rescue place at the Dak Lak Elephant Conservation Center in Vietnam. During the following months he became accustomed to the presence of humans by positive reinforcement training. The wounds were taking care of by daily flushing with saline and antiseptic (povidone-iodine solution) solutions. Arrangements could be made to make X-rays of the affected leg, which revealed the piece metal wire. During a surgery under general anesthesia (ketamine and xylazine by IM-injection and oxygen supplementation in the trunk), a 20 cm of wire was removed. The incision was made perpendicular on the wire until the scalpel touched the wire. By slightly enlarging the wound the wire was easily removed. The wound was left open and flushed daily during the following weeks (saline and antiseptic solutions). The incision wound healed restless. Three of the 4 initial fistulas closed in the following year.




However, one fistula located at the medio-palmar side of the circular scar remained oozing. Seven months after the removal of the wire, there was an opportunity again to inspect the wounds and radiographs were made again. Based on these images osteolysis of one of the carpal bone was suspected. A second surgery was done and pieces of smelling necro-purulent bone material were removed by cutting the affected carpal bone using a bone chisel and bone scraper. A large tunnel between the incision wound and the original wound was created in order to allow easy draining of necro-purulent exudate during the daily flushings. The surgical wound and fistula healed completely.

To date (2025) the original wound is still being managed by weekly cutting away excessive horn and daily flushing. The animal can walk reasonably well. The episodes of displaying stereotypic behavior have significantly reduced in frequency and intensity.



Several examples of a prosthesis can be found on the internet. Most of the victims lost part of the leg by the explosion of a land mine they stepped on.

Chhouk, an Asian elephant in Laos has been living for several years with a prosthetic device (See also : Wildlife Alliance)
Prevention of orthopedic problems
Management-related factors play a major role in the development of foot problems. Two studies (one performed in European zoos and one in Nort-American zoos) found the following factors influencing one or more orthopedic issues (Wendler 2019; Miller 2016):
-
Enclosure size: the larger the enclosure, the less problems occurred.
-
Bedding: soft bedding reduced the number of orthopedic problems.
-
Floor: a dry floor promotes foot health
-
Time spend outdoor: the longer an elephant spends time in its outdoor enclosure, the better it is for its locomotion apparatus
-
Exercise: adequate exercise by many social interactions reduces orthopedic issues
-
Provide a headrest (see under 'treatment')
-
Nutrition: more brows results in less foot problems. Benz (2005) could not find a correlation between the supplementation of the diet with biotin (vitamin B8) and foot health.
-
Body condition: no negative correlation was found between overweight and orthopedic problems.
Elephants that are kept in range countries are facing different management-related issues. Walking large distances on hot tar roads may result in damage to the pad. Elephants working in the logging industry may be more affected by muscle or joint injuries. As many elephants are not trained for foot care, easy-to-treat nail or pad lesions may lead to complications like foot abscesses or osteolysis of the distal phalanges. However, no data are available about the incidence of foot problems in range countries.
A separate chapter about regular foot care in elephants kept in zoos can be found here.
Stereotypical behaviors like "weaving (or swaying)" may result in excessive pressure on the lateral nails resulting in cracks. This stresses the importance of providing a divers social setting for elephants to live in, mimicking their natural social environment.
Training of elephants to allow proper foot care is important to address early problems of foot lesions. Mahouts should have the minimum knowledge and skills to perform proper foot care. In order to monitor the effect of pedicure, it is important to describe the status of the feet. By clicking on the icon displayed below, you will find a document that can be used for this purpose (from EAZA Best Practice Guidelines for Elephants, 2020):
Click here to download the foot examination form for Asian elephants
Click here to download the foot examination form for African elephants
No studies about the prevention of degenerative joint disease have been published. As the cause of this problem in elephants is not known, it is hard take appropriate measures to prevent them. Without hard evidence some more anecdotal statements may still be useful:
-
Provide sand piles for sleeping during the night
-
Stimulate locomotion (free ranging elephants walk many miles per day!)
-
Provide sufficient soft bedding.
Further reading: see reference list.
References
-
Abbondanza, F.N., Power, M.L., Dickson, M.A., Brown,B. and Oftedal O.T. 2013. Variation in the Composition of Milk of Asian Elephants (Elephas maximus) Throughout Lactation. Zoo Biology 32(3):291-8.
-
Benz, A. 2005. The elephant’s hoof: Macroscopic and microscopic morphology of defined locations under consideration of pathological changes. Master's thesis, Veterinary Faculty of the University Zürich, Switzerland.
-
Clark H. W., Laughlin D. C., Bailey J. S. and Brown T. McP. 1980. Mycoplasma Species and Arthritis in Captive Elephants. Journal of Zoo Animal Medicine, Vol. 11, No. 1 pp. 3-15.
-
Csuti B, Sargent E.L., Bechert U.S. (Editors) 2005. Book: The Elephant's Foot: Prevention and Care of Foot Conditions in Captive Asian and African Elephants 1st Edition.
-
EAZA Best Practice Guidelines for Elephants. 2020. Click here for full text.
-
Elze K. 1962. Über eine unter dem klinischen Bild van Botulismus verlaufene Erkrankung beim Elefanten. Nord.Vet.-Med. 14 (1) 259-271.
-
Fowler M.E. and Mikota S.K. 2006. Biology, Medicine, and Surgery of Elephants. 271-290.
-
Hess A. 2022. Lesions found in the post-mortem reports of the Asian (Elephas maximus) and African (Loxodonta africana) elephants of the European Association of Zoos and Aquaria Master's thesis, Department of Exotic Animal and Wildlife Medicine University of Veterinary Medicine Budapest, Hungary.
-
Johnson G., Smith J., Peddie J., Peddie L., DeMarco J., Wiedner E. 2018. Use of glue-on shoes to improve conformational abnormalities in two Asian elephants (Elephas maximus). J. Zoo&Wildl Med. 49(1): 183–188, 2018.
-
Karunarathne H.P.R.N.S., Bandara M.R.B.N., AbeysingheA.M.N.D.B.,Liyanage E.M.E., Rajapaksha R.C., Kodikara D.S. and Dangolla A.. 2017. Fixation of a Radius and Ulna Fracture in an Asian Elephant Calf by Using Fibreglass Casts. Gajah 47 (2017) 40-41.
-
Kottwitz J, Bechert U, Cruz-Espindola C, Christensen J.M., and Boothe D. 2024. Single-dose, multiple-dose, and therapeutic drug monitoring pharmacokinetics of firoxicab in Asian elephants (Elephas maximus). Journal of Zoo and Wildlife Medicine 55(1): 73–85, 2024.
-
Miller M.A., Hogan J.N., Meehan C.L. 2016. Housing and Demographic Risk Factors Impacting Foot and Musculoskeletal Health in African Elephants [Loxodonta africana] and Asian Elephants [Elephas maximus] in North American Zoos. PLoS ONE 11(7): e0155223. doi:10.1371/journal.pone.0155223.
-
Schiffmann C. 2021. Posture Abnormalities as Indicators of Musculoskeletal Disorders in 12 Zoo Elephants – a Visual Guide. Gajah 53 (2021) 20-29.
-
Turner A., Masters N., Pfau T., Hutchinson J.R., and Weller R. 2023. Development and evaluation of a standardized system for the assessment of locomotor health in elephants under human care. J. Zoo&Wildl Med. 54(3): 529-537.
-
Wendler, P., Ertl, N.,Flügger, M., Sós, E., Schiffmann, C., Clauss, M., and Hatt,J-M. 2019. Foot health of Asiane elephants (Elephas maximus) in European zoos. Journal of Zoo and Wildlife Medicine 50(3): 513–527, 2019.

